Why is it so hard to make a doctor's appointment as a healthcare worker?
Or in other words, why is it so difficult to be a patient?
Dear Friends,
Without conferring,
and I chose the same exact artist’s date this week: seeking medical care. Is it sad that this is our version of ‘two hours weekly, especially set aside and committed to nurturing your […] inner artist?” Maybe. And yet, as artists, we still have bodies, that require checkups and things to stay healthy so we can keep being our creative forces in the world!It isn’t the most straightforward form of logic but this line of reasoning helped me cross the chasm from I know I should make a PCP appointment to picking up the phone, waiting on hold, hearing everyone has quit primary care (surprise, surprise), nobody is accepting new patients, and finally that I indeed can be seen in three months (which by then I will have new insurance again so will likely have to start the process over again).
For the record, this matching artists’ date was not planned.
But it has led me to reflect on why it was so particularly difficult for both of us, two healthcare girlies, to prioritize our medical care. I wonder, nonetheless, is it just me? I think it’s likely a combination of things, so bear with me while I recklessly posit some reasons it could be:
Depersonalization. Depersonalization in healthcare refers to a psychological state where providers begin to treat patients as objects or cases rather than as individuals with unique needs and emotions. Further, we can understand it as a failure of compassion in the face of overwhelming strain. It serves as a defense mechanism, rooted in the desire to reduce vicarious harm, allowing healthcare providers to shield themselves from the emotional burden of engaging with every story of pain they encounter. I wonder if this attempt to place an increased distance between ourselves and our patients makes it particularly difficult for us to cross to other side of becoming a patient. Furthermore, depersonalization involves a sense of emotional numbness or detachment. With a practice numbness, we may struggle to recognize or validate our own emotional and physical needs, making it harder for us to acknowledge when they require medical care.
Codependency. In nursing school, my Med-Surg professor suggested we all reflect on whether we may be on the spectrum of codependency considering our decision to become nurses: a life dedicated to caring for others’ needs. From my own experience, I believe many of us HCWs gain our sense of self-worth from caring or serving for others. As Introspective Spaces collaborator, Gina Ryder, explains in a recent LifeKit episode , codependency is when caring veers into caretaking, prioritizing others’ needs above your own, and betraying your own needs in service of others. An adaptive pattern often established in trauma, it becomes maladaptive when we’ve become so good at erasing our own needs that we cannot hear or sense them anymore. In nursing, we wear this as a badge of honor. I didn't pee all day! It can show up in more insidious ways such as tolerating unprofessional behavior from patients or colleagues, an intense need to be validated by patients or colleagues, fear of delegating tasks, and taking on responsibility for a patient’s outcome. Healthcare work can be so absorbing that we have the perfect and very important excuse to not return to ourselves because, well, someone was literally dying, so I had to stay late, pick up the shift, skip my break, or cancel my OB appointment.
The Patriarchy. Even when women earn more than their hetero partners, they take on, on average, 3.5 more hours of household work and caregiving at home per week. That’s 3.5 hours less time a week to take care of oneself. Even if women are unpartnered, they often end up doing more ‘unpromotable’ work such as taking on emotional labor, such as mediating conflicts, offering support to colleagues, and remembering important dates and milestones. These responsibilities, while valuable, often go unnoticed and unrecognized, further perpetuating the imbalance in both professional and personal spheres. If I do have a spare hour, let’s be honest, I’m probably going to choose something that has more short-term satisfaction like getting a latte or reading a book.
Over-identification. We viscerally know what our providers are going through so we don’t want to be an added ‘burden’ to what we know is already an uphill battle. For example, we know our PCP does not have time during the day to respond to MyChart messages. So what do we do? Stay silent, stay quiet, try to handle our health issue on our own (or is that just me?).
I do not want to go to there. As Eva Tuchman Leonard uncomfortably points out in her recent book, Bodywork “anything that can happen to a human can also happen to me.” This is something we spend a lot time running from as HCWs because frankly, it’s terrifying. We see a lot of really awful things happen to human bodies. Usually we see those awful things happen at the clinic or hospital. So I would rather not go to there.
I think for me, it’s a big serving of codependency, a dash or moral distress, with a cherry on top of living under the patriarchy. This really turned into a bit of a downer! The obstacles in our path back to prioritizing our own needs are legion. That being said, I think there are many ways around and over and through and I think the Artist’s Way is one of those that happened to be highly effective for myself (and Sarah!). And perhaps it’s not even the Artist’s Way as a silver bullet, but rather building the muscle of self-accountability and care in community, the structure of the mirrored face of our colleagues and friends celebrating the large and small wins with us of making a doctor’s appointment.
You’ve most certainly had this conversation (rant?) with your friends so please tell me what did I miss? We’d love to hear from you!
Till next time,
Laura and Anu
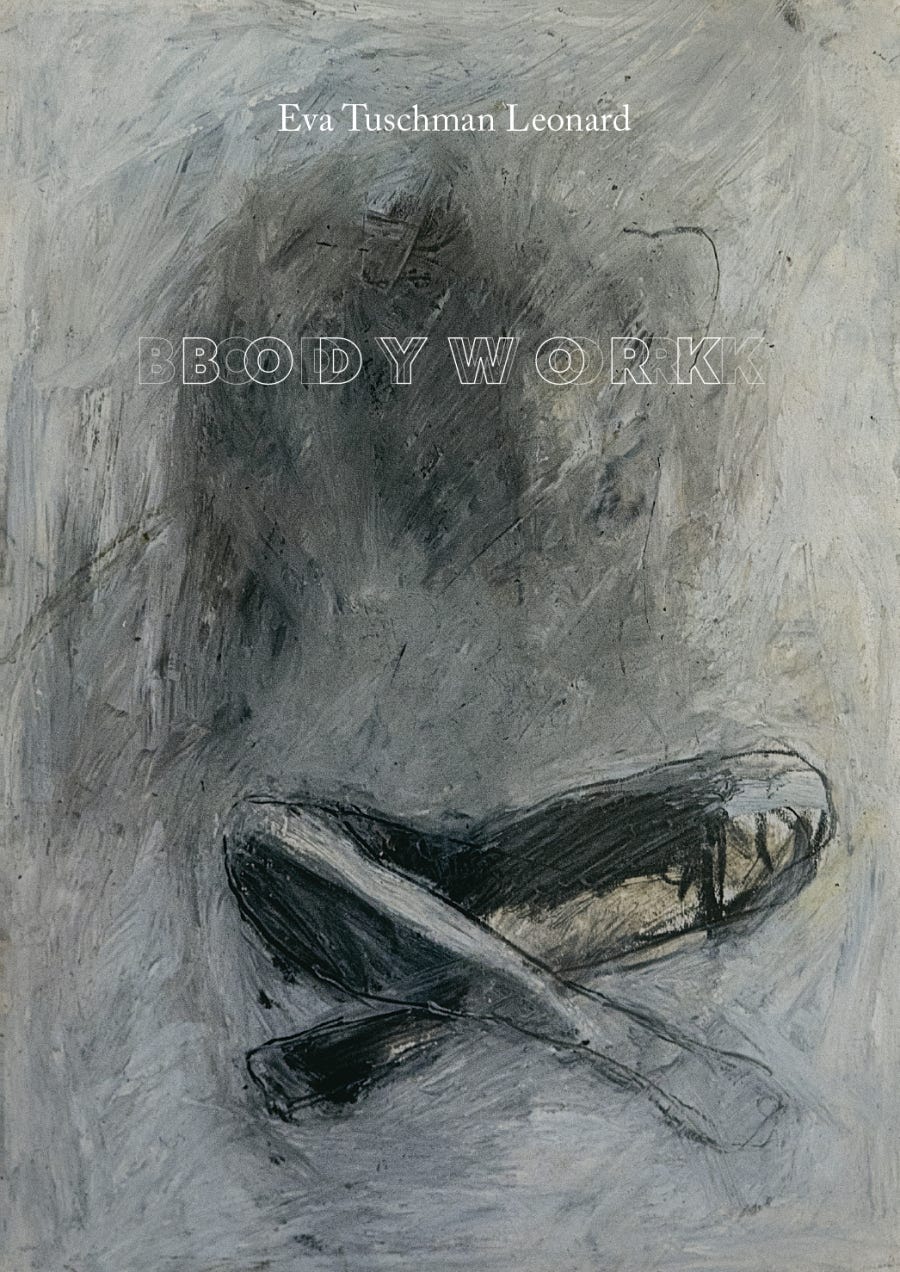
Bodywork
“the body is our first and final home”
Speaking of tending to our physical bodies: Bodywork, Eva Tuschman Leonard takes readers on a deeply personal journey that intertwines art, memory, and the physical body. Through a blend of drawings, prose, and fragments, Leonard revisits her younger self—full of vitality and creative energy—and contrasts it with her current experience of living with autoimmune disease. As she unearths a forgotten archive of self-portraits, she’s struck by how these early works, with their depictions of unraveling bodies, seem to foreshadow the physical challenges she now faces. Bodywork invites us to contemplate the coexistence of pain and joy within a single body, and the ways in which our art can sometimes reveal truths we aren’t yet ready to see.
Click the image below to learn more! And if you are planning on attending our upcoming retreat in Los Angeles in the winter (December 8, mark your calendar!) we will have copies available.
Registration is open!
We are so excited to offer The Artist’s Way for the healthcare worker community!
TWO MORE WEEKS TO SIGN UP! The earlier you sign up the earlier we can match you to a group.
The Artist’s Way is a twelve week workbook to reconnect with your inner artist through play, reflection, exercises, and examining our inner beliefs about our creativity.
Anu and I have been inspired by our experience with the Artist’s Way. We see this as an important tool in unblocking our own creativity, healing our imagination, so we can reimagine a new way forward into healthcare together.
We will be offering this to individuals in our community, but we are also seeking clinics, units, and workplaces who may have more than one person interested so we can form a pod at that institution for a discounted rate.
Registration is now open! Sign up here!